It keeps getting worse and worse!
Why are Black maternal mortality rates so high?
“Even the healthy women — such as decorated U.S. Olympic sprinter Tori Bowie — can die from complications of childbirth.”
Dozens of pregnant women, some bleeding or in labor, are turned away from ERs despite federal law
“WASHINGTON (AP) — Bleeding and in pain, Kyleigh Thurman didn’t know her doomed pregnancy could kill her.
Emergency room doctors at Ascension Seton Williamson in Texas handed her a pamphlet on miscarriage and told her to “let nature take its course” before discharging her without treatment for her ectopic pregnancy.
When the 25-year-old returned three days later, still bleeding, doctors finally agreed to give her an injection to end the pregnancy. It was too late. The fertilized egg growing on Thurman’s fallopian tube ruptured it, destroying part of her reproductive system.”
“More than 100 pregnant women in medical distress who sought help from emergency rooms were turned away or negligently treated since 2022, an Associated Press analysis of federal hospital investigations found.”
Infant mortality in the US rose 3% in 2022, marking 1st significant increase since 2002: CDC The infant mortality rate was 5.61 deaths per 1,000 live births in 2022.
I wonder what could have caused this? A great read:

It has a report:

“EXECUTIVE SUMMARY Every year in the United States, around 700 mothers die, and 60,000 suffer from pregnancy-related diseases or medical conditions (March of Dimes, 2020). And yet, this is a complicated problem that varies widely depending on where a person lives: the risk of dying from maternal causes differs from state to state, and the leading causes for poor outcomes differ by age, race, and timing of death. What’s more, empirical evidence has found that risk factors are more prevalent and outcomes are far worse for Black, American Indian/Alaska Native, and rural mothers.”
“the risk of dying from maternal causes differs from state to state” – I have maps – Red States vs Blue States (Blue is good in my maps)
Medicaid Expansion: What’s the Status in Your State?
Which states have not expanded Medicaid?
Ten states — Alabama, Florida, Georgia, Kansas, Mississippi, South Carolina, Tennessee, Texas, Wisconsin, and Wyoming — have not accepted the Medicaid expansion.
In his January State of the State address, Mississippi Gov. Tate Reeves urged legislators to reject expanding the program.“Don’t simply cave under the pressure of Democrats and their allies in the media who are pushing for the expansion of Obamacare, welfare and socialized medicine,” Reeves said. “Instead, seek innovative free market solutions that disrupt traditional healthcare delivery models, increase competition, and lead to better health outcomes for Mississippians.””
What color are Alabama, Florida, Georgia, Kansas, Mississippi, South Carolina, Tennessee, Texas, Wisconsin, and Wyoming on these maps?
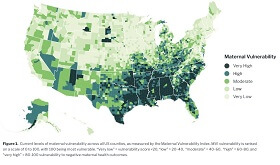
The Surgo report has this information:
“It can help inform new legislation at federal, state, and local levels. Though the US government has crafted policy responses to this challenge, much of the proposed legislation has been held up in Congress. The legislation that has passed through state legislatures has been patchy and inconsistent. The MVI can help to determine which pieces of legislation are most necessary, and in what geographies, thereby sharpening legislative focus.”
Surgo has a map – see a pattern?

The March of Dimes gave me a plaque once for organizing a Coed Softball Tournament to raise money for the organization.

2023 March of Dimes report card for United States
March of Dimes has Maps – see the pattern?

Maternal mortality rate is going UP! The Dobbs Decision will increase this even more!

Louisiana woman whose water broke at 16 weeks was forced into ‘painful, hours-long labor’ because of abortion ban, lawsuit says
“A Louisiana woman experiencing a miscarriage at 16 weeks of pregnancy was forced to endure a painful, bloody, and traumatizing labor and delivery, according to a sworn affidavit from her OB/GYN, after she was denied a simple 15-minute procedure due to the state’s abortion ban.
“She was already traumatized from her experience and felt that an induction, which would require labor and delivery of the fetus, would be too much for her,” Dr. Valerie Williams said in court documents obtained by Insider.
But the hospital’s lawyer immediately told Williams she couldn’t perform the D&E due to Louisiana’s trigger ban.
“Going back into that hospital room and telling the patient that she would have to be induced and push out the fetus was one of the hardest conversations I’ve ever had,” Williams said.”
Louisiana doctors detail unintended consequences of state’s abortion ban
“”I am more likely to die than my mother was in childbirth. So as a country, our outcomes are getting worse,” Dr. Rebekah Gee, an OB-GYN and a former secretary of the Louisiana Department of Health, told 60 Minutes.”
In Louisiana, pregnant women struggle to get maternal health care, and the situation is getting worse
“The United States is in the middle of a maternal health crisis. Today, a woman in the U.S. is twice as likely to die from pregnancy than her mother was a generation ago.
Statistics from the World Health Organization show the United States has one of the highest rates of maternal death in the developed world. Women in the U.S. are 10 or more times likely to die from pregnancy-related causes than mothers in Poland, Spain, or Norway.
As we first reported this past April, some of the worst statistics come out of the South – in places like Louisiana, where deep pockets of poverty, health care deserts and racial biases have long put mothers at risk.”
See a pattern yet? “some of the worst statistics come out of the South – in places like Louisiana”


We are trailing the rest of the industrialized world!
Insights into the U.S. Maternal Mortality Crisis: An International Comparison
“Introduction
The United States continues to have the highest rate of maternal deaths of any high-income nation, despite a decline since the COVID-19 pandemic. And within the U.S., the rate is by far the highest for Black women. Most of these deaths — over 80 percent — are likely preventable.1
With policies and systems in place to support women during the perinatal period, several high-income countries report virtually no maternal deaths. As policymakers and health care delivery system leaders in the U.S. seek ways to end the nation’s maternal mortality crisis, these countries may offer viable solutions.”
Highlights
- In 2022 there were approximately 22 maternal deaths for every 100,000 live births in the United States — far above rates for other high-income countries. U.S. maternal mortality is lowest for Asian American women and highest for Black women.
- Maternal death rates increased in Australia, Japan, the Netherlands, and the U.S. during the height of the pandemic, between 2020 and 2021. In Chile, Norway, and the U.S., where 2022 data are available, maternal death rates have begun to decline.
- Nearly two of three maternal deaths in the U.S. occur during the postpartum period, up to 42 days following birth. Compared to women in the other countries we studied, U.S. women are the least likely to have supports such as home visits and guaranteed paid leave during this critical time.
- The U.S. and Canada have the lowest supply of midwives and ob-gyns. In the U.S., Canada, and Korea, ob-gyns outnumber midwives.”
“Recent Maternal Mortality Trends”

“In 2022, there were 22 maternal deaths for every 100,000 live births in the U.S. — more than double, sometimes triple, the rate for most other high-income countries in this analysis. In half of the countries, there were less than five maternal deaths per 100,000 live births.
For Black women, maternal mortality is exceptionally high. Prior research has found Black people receive worse-quality care than white people on 52 percent of measures, including measures of care process, such as the ability to receive needed care; care outcomes, such as death; and patients’ perceptions of care.3
Other data show that racial disparities exist both within hospitals and between hospitals for maternal morbidity.4 Inequities in access to care and patients’ experience of care are often rooted in discrimination and clinician bias.5“

“In Chile, Norway, and the U.S., for which 2022 data are now available, the maternal death rate has begun to decrease once again. In 2022, Norway’s maternal mortality rate was 0.11“

“Differences in Care During Pregnancy, Labor, and Delivery”

“Midwives are clinicians trained to provide a wide range of services — helping to manage normal pregnancies, assisting with childbirth, and providing care during the postpartum period, among others. In many countries, they are key providers of reproductive health care for women. A recent study found that a midwife workforce, integrated into health care delivery, could provide 80 percent of essential maternal care around the world and potentially avert 41 percent of maternal deaths, 39 percent of neonatal deaths, and 26 percent of stillbirths.13 By placing a priority on natural reproduction processes and relationship-building, midwives also can help address the social needs of mother, baby, and family.14
Midwifery-led care models have been shown to provide care that is comparable to, or sometimes even better than, that provided by obstetrician-gynecologists, or ob-gyns.15 In the U.S., Canada, and Korea, ob-gyns outnumber midwives, while in most other countries midwives greatly outnumber ob-gyns.
The U.S. and Canada have the lowest overall supply of midwives and ob-gyns — 16 and 13 providers per thousand live births, respectively. Nearly 7 million women in the U.S. currently live in counties where there are no hospitals or birth centers offering obstetric care and no obstetric providers, and the shortage is expected to only get worse in coming years.16“

“High-quality postpartum care is intended to ensure the physical and emotional recovery of mothers and their babies and can help reduce maternal deaths.17 Visits by a midwife or a nurse are associated with improved mental health and breastfeeding outcomes as well as reduced health care costs. Home visits give providers an opportunity to address maternal and mental health concerns as well as to assess the mother’s available supports and social drivers of health, including needs for food, housing, financial security, and protection from domestic violence.
All countries, apart from the U.S., guarantee at least one such home visit within one week postpartum, although Medicaid programs in some U.S. states cover these visits.”

Child support at Conception? The and Evangelists profess to love babies BEFORE they are born, but once they ARE born they could care less about their healthcare, nutrition, housing, safety or freedom. Pro-Life = Pro-Birth-to-Pander-For-Votes

Remind me again which political party IS pro-life?








They have a map